
Penelope Petrie is a retired teacher and a lifelong learner. Penelope is a volunteer with several organizations in Hamilton and McMaster University that focus on issues impacting older adults. She joined the Collaborative because it offers several opportunities to learn about aging research, influence health policy, and promote healthy aging. Penelope’s goal is to ensure best practices are being implemented in communities in need.
Fun Facts
Hometown: Hamilton, ON
Favourite colour: Red
Hidden talent: I can fly an airplane
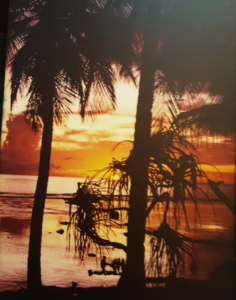
Bucket list item: Return to visit Pingelap Island, Pohnpei, Micronesia (Carolina Islands)
Most prized possession: My education
Image: View of the sunset overlooking the reef from my window, Pingelap Island, Pohnpei, Micronesia (Carolina Islands).
Photo credit: Penelope Petrie
What do you enjoy most about being a partner at the Collaborative?
I’d say it’s the opportunity to meet young researchers — people who are in the early stages of their career. Just the enthusiasm that these people have for doing research and learning research methods. It’s so inspiring.
What does “aging well” mean to you as an older adult? How has this differed as a child or young adult?
To me, it means being healthy and having the physical, emotional and financial resources to live and do the things that I want to do, but also accepting my limitations as they arise. Because, to me, being able to live my life as I wish, being able to stay in my home, to do the traveling that I want to — that’s aging well. And to not worry about having this taken away. I intend to live where I am now for the rest of my life, if possible.
And part of aging well, to me, is also keeping busy. I do a lot of volunteer work. I find it enjoyable. Just having those opportunities is important to me.
As a child or even as a younger adult, I don’t think that I ever really thought about getting old. You know, it just sort of creeps up on you and then, all of a sudden, you think “Oh, gee, I’m in that age group that they’re talking about.” I mean, I don’t see myself as old. But if I get to the point where I am having these restrictions imposed upon me — and I hope I don’t…or at least not for a long time — then I think I’ll start to feel old.
If you could change one thing about the services and supports in healthcare that are available to older adults, what would it be?
Access to homecare would be a big one for me, because I think that I’m not alone in terms of wanting to stay where I am, the home that I live in. People don’t necessarily want to move into what others may think are “appropriate” alternate home care settings. That may mean that you will need adequate supports to stay in your own home — perhaps in the form of a lift or a wheelchair — to be able to move around within and out of the house, but still allow you to stay in your home.
Another worry of mine is access to a family doctor. My family doctor has declared that he has a five-year plan to retire. What will happen then? It is now very difficult to find a doctor who will take you on as a new patient, and in some cases, more difficult, as an older adult. I know this because when my family doctor decided to leave family medicine and change their area of focus, I tried pretty much every doctor in Hamilton who was accepting new patients. I got asked two questions when I called to see if I could come in and talk to the doctor: my name and my age. And I didn’t fit anybody’s practice based on that information.
I’m also concerned about health care privatization. Many older adults are on extremely fixed incomes. For example, going to a private clinic where you have to make a payment may not be possible because they don’t have the finances to do so. And then there’s inflation, which will potentially include the cost of basic health care going up, that those on a fixed income will not be able to budget for.
What advice would you give to researchers who are interested in partnering with older adults in aging-focused research?
Go for it! And listen. Really listen.
And my other piece of advice that I often give is, try not to use jargon and acronyms. Older adults may not know, understand, or remember the jargon but we have a lifetime of experience and ideas to offer. It can be very demoralizing, you know. These terms that are being thrown around as part of the conversation, and I’m thinking “Everybody in this room knows what that is, but me.”
Creating that inclusive space that allows everybody to feel like they belong is important. And sometimes, you may need to remind people of that because it could be the difference in how your partners contribute to the work you do as a researcher.
What three words would you use to describe your experience within the Collaborative?
Worthwhile, enjoyable and educational.
